Crusted scabies is a less common but more severe form of scabies, characterized by distinct clinical and pathological features compared to common scabies. It presents with a more severe disease course, a shorter incubation period, and a prolonged treatment duration.1 This condition is often observed in predominantly immunocompromised individuals, the elderly, or those with neurological impairments such as Parkinson’s disease, post-stroke limb weakness, and comorbidities such as diabetes mellitus or chronic malnutrition. Clinically, crusted scabies can mimic other dermatological conditions, including atopic dermatitis, psoriasis, and seborrheic dermatitis. This clinical overlap frequently leads to diagnostic delays, resulting in prolonged patient suffering and significantly reduced quality of life.2
Various tools are available to diagnose crusted scabies, such as dermoscopy, potassium hydroxide (KOH) preparations of scabies mites, and skin biopsies from affected areas.3 However, skin biopsy poses challenges as the preferred sites for infestation, such as the hands and genitals, are often sensitive and prone to painful, slow-healing ulcers post-biopsy.
Systemic therapy is typically considered the first-line treatment for crusted scabies, with ivermectin being the most commonly used medication. However, systemic treatments can produce adverse effects that may be poorly tolerated, particularly in populations predisposed to crusted scabies.2
In this report, we present two cases of crusted scabies, discussing our clinical experience and highlighting an alternative approach to diagnosis and treatment in this challenging condition. Informed consents were obtained from the patients for publication.
Case one
A 70-year-old male patient presented with erythema on his back and chest, accompanied by small papules on his chest and extremities that rapidly developed into yellow scaling lesions. His symptoms began approximately one month before presentation to our hospital. He had poorly controlled type 2 diabetes. Initially misdiagnosed with atopic dermatitis, he was treated with topical corticosteroids. However, his condition worsened, with increased itching and scaling [Figure 1a and b].
Based on clinical suspicion of crusted scabies, we administered a KOH treatment to his hand and performed a skin biopsy surrounding the umbilical region. Scabies mites were negative on KOH preparation but were identified in the biopsy specimen [Figure 1c]. We did not conduct a dermoscopy examination for scabies as this is not available at our hospital.

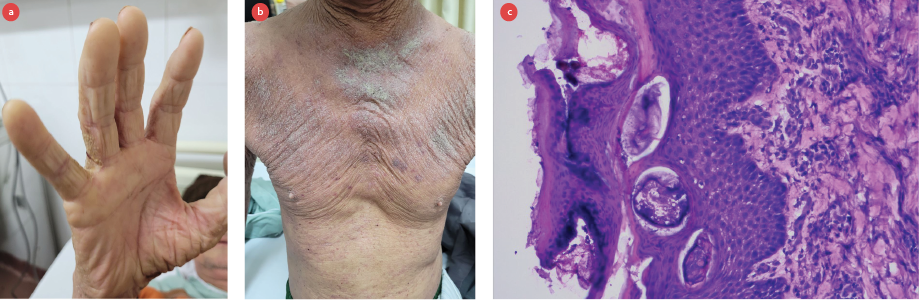 Figure 1: (a) Pruritic, thick, hyperkeratotic, yellow-crusted plaques observed in the interdigital spaces (webbing) of the fingers. (b) Thick, erythematous, diffusely scaling plaques present on the chest. (c) Histopathological examination showing marked hyperkeratosis with parakeratosis in the stratum corneum. The epidermis shows acanthosis and spongiosis, with numerous mites and eggs, and a mild superficial perivascular lymphocytic infiltrate (hematoxylin and eosin, magnification = 20 ×).
Figure 1: (a) Pruritic, thick, hyperkeratotic, yellow-crusted plaques observed in the interdigital spaces (webbing) of the fingers. (b) Thick, erythematous, diffusely scaling plaques present on the chest. (c) Histopathological examination showing marked hyperkeratosis with parakeratosis in the stratum corneum. The epidermis shows acanthosis and spongiosis, with numerous mites and eggs, and a mild superficial perivascular lymphocytic infiltrate (hematoxylin and eosin, magnification = 20 ×).
The patient was treated with permethrin 5% cream, applied the entire body, and repeated one week later. The response to treatment was excellent, with complete resolution of itching and scaling within two weeks, indicating full recovery.
Case two
A 76-year-old male presented with a two-month history of generalized xerosis, mild desquamation, and thick yellow-green crusted plaques with malodor, localized to his right hand [Figure 2a]. He had a 12-year history of post-stroke limb weakness and functional dependence, resulting in compromised self-hygiene. An initial misdiagnosis of psoriasis by a primary care clinician led to treatment with betamethasone-salicylic acid ointment, which yielded no clinical improvement.
A dermatological re-evaluation raised suspicion of scabies. Diagnostic workup included a KOH preparation and punch biopsies from two sites: the right forearm and periumbilical skin. Microscopic examination of the KOH preparation revealed Sarcoptes scabiei mites [Figure 2b], and histopathology of the periumbilical biopsy confirmed the scabies infestation [Figure 2c]. No mites were identified in the forearm biopsy.

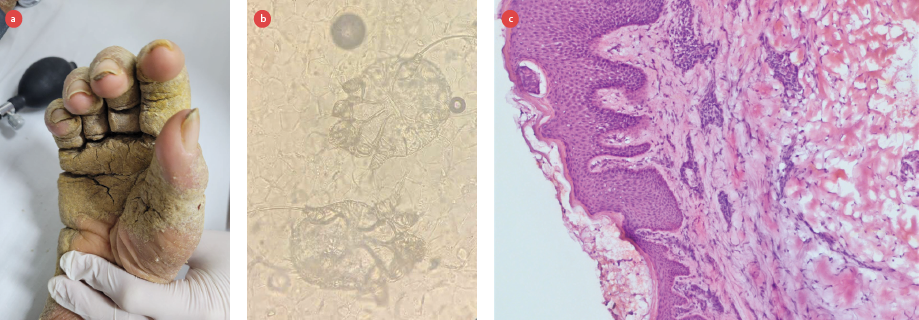 Figure 2: (a) Thick, diffuse hyperkeratotic yellow-green plaques with adherent scales covering the dorsal and palmar surfaces, including pronounced crusting in the interdigital spaces, areas of fissuring, mild erythema beneath the thick scales, and nail subungual hyperkeratosis. (b) A potassium hydroxide preparation 40 revealed adult scabies mites, magnification = 40 ×. (c) Hematoxylin and eosin staining shows significant hyperkeratosis in the stratum corneum, magnification = 20 ×. The epidermis exhibits acanthosis and spongiosis, with a mite located just beneath the stratum corneum, and mild superficial perivascular lymphocytic infiltration.
Figure 2: (a) Thick, diffuse hyperkeratotic yellow-green plaques with adherent scales covering the dorsal and palmar surfaces, including pronounced crusting in the interdigital spaces, areas of fissuring, mild erythema beneath the thick scales, and nail subungual hyperkeratosis. (b) A potassium hydroxide preparation 40 revealed adult scabies mites, magnification = 40 ×. (c) Hematoxylin and eosin staining shows significant hyperkeratosis in the stratum corneum, magnification = 20 ×. The epidermis exhibits acanthosis and spongiosis, with a mite located just beneath the stratum corneum, and mild superficial perivascular lymphocytic infiltration.
The patient was treated with topical permethrin 5% cream applied to the entire body, repeated after one week. Adjunctive keratolytic therapy with salicylic acid was administered to reduce hyperkeratosis. Scaling and pruritus was resolved within two weeks, with complete eradication of the infestation confirmed at follow-up.
Conclusion
Hyperkeratosis of the palms characterized by thick yellow or yellow-green crusts, may serve as a valuable diagnostic clue for distinguishing scabies from other generalized desquamating disorders. A biopsy of the periumbilical region can be considered as a potential diagnostic site for confirming scabies infestation. Finally, topical permethrin 5% therapy represents an effective alternative for managing scabies in patients who have contraindications or intolerance to systemic ivermectin therapy.
Disclosure
The authors declare no conflicts of interest.
references
- 1. Niode NJ, Adji A, Gazpers S, Kandou RT, Pandaleke H, Trisnowati DM, et al. Crusted scabies, a neglected tropical disease: case series and literature review. Infect Dis Rep 2022 Jun;14(3):479-491.
- 2. Uzun S, Durdu M, Yürekli A, Mülayim MK, Akyol M, Velipaşaoğlu S, et al. Clinical practice guidelines for the diagnosis and treatment of scabies. Int J Dermatol 2024 Dec;63(12):1642-1656.
- 3. Siddig EE, Hay R. Laboratory-based diagnosis of scabies: a review of the current status. Trans R Soc Trop Med Hyg 2022 Jan;116(1):4-9.