The thyroid gland originates from the invasion of midline endodermal cells during the third and fourth weeks of embryological development. An epithelial invagination descends along the midline from the base of the tongue to the front of the neck, forming the thyroglossal tract.1 The hyoid bone develops from the mesoderm of the second and third arches, allowing the thyroglossal tract to pass ventral to it. Between the eighth and 10th week of gestation, the thyroglossal duct obliterates. The thyroglossal cyst is caused by the inability to obliterate portions of this canal completely, presents in 7% of individuals with midline swelling.2
Thyroglossal duct cysts (TGDCs) typically present in the neck as asymptomatic midline swellings, with lateral occurrences reported rarely.3 Fewer than 1% of TGDCs have concurrent thyroid cancer that develops in an untreated cyst.4 Signs of cancer include dysphagia, dysphonia, and gradual weight loss with a rapid increase in the tumor size. Most patients are asymptomatic, with a median age at diagnosis of 40 years.5 Fine-needle aspiration cytology often yields false negatives, making histological examination crucial for accurate diagnosis. Due to the rarity of carcinoma, there are no set standards for a typical treatment plan.3
Case report
A 25-year-old female presented with a three-month history of swelling and pain in the left lateral neck, exacerbated during eating. On examination, a 4–5 cm enlargement in the left lateral neck was observed, associated with pain on swallowing and slight mobility with tongue protrusion. No thyroid enlargement or signs of hyper or hypothyroidism were noted, and cervical lymph nodes were not palpable. Routine blood work and thyroid function tests were within normal limits. Neck ultrasound revealed a cystic lesion (46 × 23 × 18 mm) in the anterior lateral neck, with the thyroid appearing normal. A radiological diagnosis of a branchial cyst was initially suggested, and further confirmation through histopathology and cytology correlation was advised. Subsequent magnetic resonance imaging confirmed the findings [Figure 1].
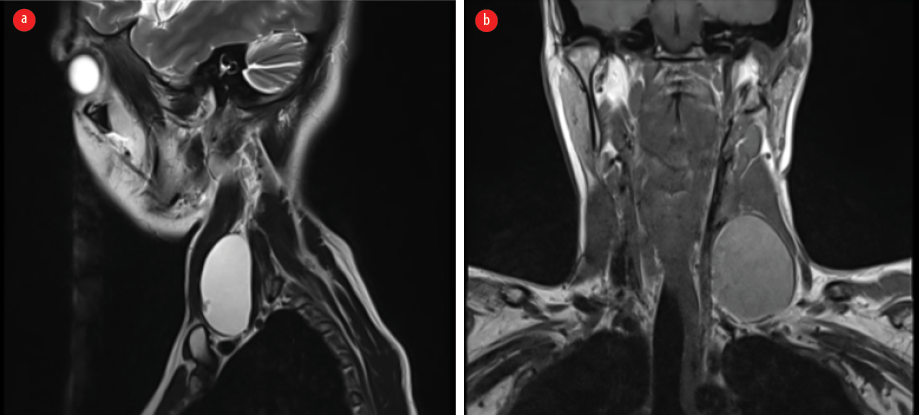 Figure 1: (a) MRI showing a heterogeneous swelling in the midline of the neck, and (b) in the left lateral part of the neck.
Figure 1: (a) MRI showing a heterogeneous swelling in the midline of the neck, and (b) in the left lateral part of the neck.
Fine-needle aspiration cytology showed a predominantly hemorrhagic and proteinaceous background, with a few mucinous flakes and tiny clusters of benign epithelial cells. Cyst macrophages were also present, suggesting a benign cystic lesion [Figure 2a and b]. Upon excision, the cyst measured 4 × 3 × 2 cm, and released 5 mL of hemorrhagic fluid. Gross examination revealed a grey-white cyst wall with papillary excrescences [Figure 3]. Histopathological examination showed columnar epithelial cells lining the cyst, along with dilated thyroid follicles containing colloid eosinophilic material [Figure 4a]. Papillary projections lined by malignant cells with eosinophilic cytoplasm, overlapping nuclei, nuclear grooves, and pale chromatin were identified [Figure 4b and c].
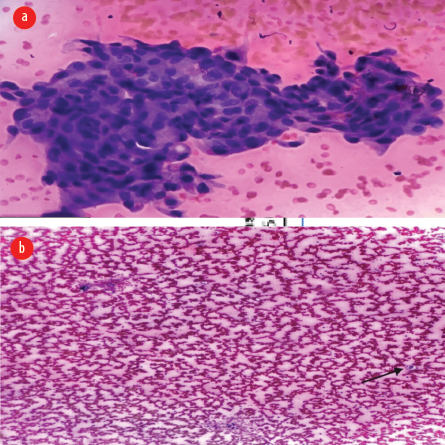 Figure 2: (a) Fine-needle aspiration cytology showing tiny clusters of benign epithelial cells and (b) tiny clusters along with cyst macrophage (black arrow).
Figure 2: (a) Fine-needle aspiration cytology showing tiny clusters of benign epithelial cells and (b) tiny clusters along with cyst macrophage (black arrow).
 Figure 3: Gross image showing papillary excrescences inside the cyst wall.
Figure 3: Gross image showing papillary excrescences inside the cyst wall.
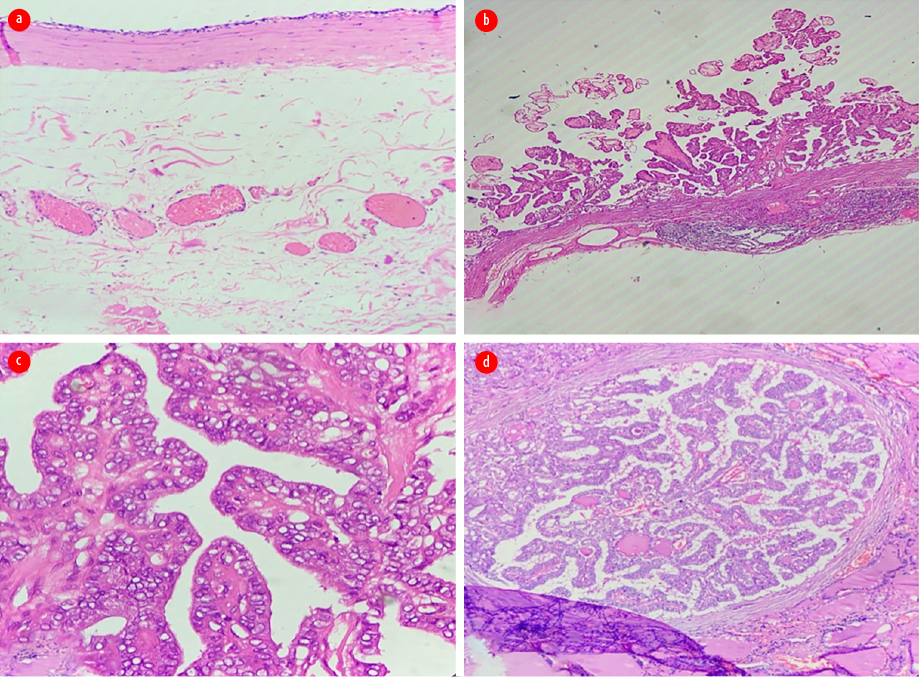 Figure 4: (a) Section from cyst wall shows benign epithelial lining, hematoxylin and eosin (H & E) magnification = 2 ×. (b) Section from cyst wall showing papillary projections that are lined by malignant cells, H & E magnification = 4 ×. (c) High power view showing classical papillary carcinoma nuclear features, H & E magnification = 40 ×. (d) Section from thyroid showing small focus of papillary carcinoma in the thyroid, H & E magnification = 10 ×.
Figure 4: (a) Section from cyst wall shows benign epithelial lining, hematoxylin and eosin (H & E) magnification = 2 ×. (b) Section from cyst wall showing papillary projections that are lined by malignant cells, H & E magnification = 4 ×. (c) High power view showing classical papillary carcinoma nuclear features, H & E magnification = 40 ×. (d) Section from thyroid showing small focus of papillary carcinoma in the thyroid, H & E magnification = 10 ×.
The patient underwent a complete thyroidectomy with radical neck dissection upon the diagnosis of primary papillary carcinoma in the lateral TGDC. The total thyroidectomy specimen, along with a radical neck dissection, was then sent for histopathological examination. The thyroid gland measured 4 × 3 × 1.5 cm, externally capsulated, and on cut section showed two tiny whitish areas in the right lobe. The thyroid gland was serially sectioned and entirely submitted for histological evaluation. Microscopy shows thyroid tissue and a small focus of papillary carcinoma in the thyroid stroma [Figure 4d]. A total of 18 lymph nodes were dissected and all were free of tumor on microscopy. The patient was discharged postoperatively and advised for follow-up.
Consent for the study and publication was obtained from the patient.
Discussion
The majority of patients with papillary thyroid carcinoma of the TGDC are asymptomatic and commonly present with dysphagia, dysphonia, increasing weight loss, and a rapidly growing mass. The median age at presentation is 40 years5. In contrast, our case involves a 25-year-old woman who presented with dysphagia due to a rapidly increasing swelling in the lateral part of her neck over three months, which was slightly movable with tongue protrusion.
Allard’s study of 381 cases of midline thyroglossal duct cysts (TGDCs) reported that the majority were infrahyoid comprising (60.9%), suprahyoid (24.1%), suprasternal (12.9%), and lingual (2.1%).6 TGDCs can manifest atypically, as demonstrated by Thabet’s study of 22 patients, where six cases presented with variable features, including intralaryngeal extension, intralingual TGDC, TGDC within the anterior neck compartment, TGDC with intracystic solid mass, inferiorly located TGDC, and laterally located TGDC.7 In our case, the swelling was present in the infrahyoid and in the left lateral aspect of the neck. Few reports in the literature described laterally located TGDCs along the anterior sternocleidomastoid muscle border and included TGDC in the differential diagnosis of branchial cleft cysts.7 In our case, the swelling was present deep to the left sternocleidomastoid muscle making it challenging to diagnose TGDC radiologically. However, it is difficult to differentiate TGDC from other cysts like brachial cysts, lymphangiomas, epidermoid cysts, dermoid cysts, and hydatid cysts clinically and radiologically.8
TGDC in the lateral aspect of the neck is rare, and TGDC developing primary carcinomas within is extremely rare, occurring in fewer than 1% of TGDC as seen in our case.3 Their cause is unknown and with no predisposing factors (i.e., neither clinical history, nor physical examination can lead to pre-operative diagnosis).9
Cytological examination obtained by fine-needle aspiration is diagnostic in onnly 66% of the cases.10 It presents similar to the benign cysts, which are the most common congenital lesion of the neck.
The pathophysiology of TGDC carcinomas has been explained by two theories: the first is direct metastasis of a papillary thyroid carcinoma and the second one is carcinoma de novo from ectopic thyroid tissue in the cyst. In our case, the thyroid gland further displayed a tiny focus of papillary carcinoma invading the thyroid stroma, making its etiology undistinguishable.9 In our case, its origin is most probably de novo, as the TGDC is present in the lateral side, having papillary carcinoma along with benign dilated thyroid follicles, and the foci of papillary thyroid carcinoma, which we found in the right lobe of the thyroid gland with no lymph node involvement.
The definitive management of TGDC carcinomas remains uncertain due to the rarity of the lesion and concerns about treatment strategies for the thyroid gland. Although some studies suggest total thyroidectomy in all cases of primary papillary carcinoma in TGDC, the optimal management strategy is not well-established.3
The atypical presentation of a TGDC is rare, and in our case, papillary carcinoma of the TGDC was present in the left lateral side of the neck, along with de novo papillary thyroid carcinoma in the right lobe of the thyroid. Such cases are infrequently reported in the literature.
Conclusion
The atypical presentation of a TGDC, particularly with coexisting papillary carcinoma, is exceptionally rare. In our case, papillary carcinoma of the TGDC was identified in the left lateral side of the neck, alongside de novo papillary thyroid carcinoma in the right lobe of the thyroid. Diagnosis typically occurs postoperatively as an incidental finding during histopathological examination. Managing these cases requires a multidisciplinary medical team to develop an appropriate treatment approach.
Disclosure
The authors declare no conflicts of interest.
references
- 1. Fernandez JF, Ordoñez NG, Schultz PN, Samaan NA, Hickey RC. Thyroglossal duct carcinoma. Surgery 1991 Dec;110(6):928-934, discussion 934-935.
- 2. Adelchi C, Mara P, Melissa L, De Stefano A, Cesare M. Ectopic thyroid tissue in the head and neck: a case series. BMC Res Notes 2014 Nov;7:790.
- 3. Gertallah LM, Eltokhy E, Baiomy TA, Harb OA. Invasive primary papillary carcinoma in a thyroglossal duct cyst: a case report and review of the literature. Hum Pathol (N Y) 2019;15:7-12.
- 4. Alatsakis M, Drogouti M, Tsompanidou C, Katsourakis A, Chatzis I. Invasive thyroglossal duct cyst papillary carcinoma: a case report and review of the literature. Am J Case Rep 2018 Jun;19:757-762.
- 5. Weiss SD, Orlich CC. Primary papillary carcinoma of a thyroglossal duct cyst: report of a case and literature review. Br J Surg 1991 Jan;78(1):87-89.
- 6. Allard RH. The thyroglossal cyst. Head Neck Surg 1982;5(2):134-146.
- 7. Thabet H, Gaafar A, Nour Y. Thyroglossal duct cyst: variable presentations. Egypt J Ear Nose Throat Allied Sci. 2011;12(1):13-20.
- 8. Taha A, Enodien B, Frey DM, Taha-Mehlitz S. Thyroglossal duct cyst, a case report and literature review. Diseases 2022 Jan;10(1):7.
- 9. Balalaa N, Megahed M, Ashari MA, Branicki F. Thyroglossal duct cyst papillary carcinoma. Case Rep Oncol 2011 Jan;4(1):39-43.
- 10. Gómez-Álvarez LR, Treviño-Lozano MA, de la O-Escamilla ME, Vergara-Miranda H, Anda LA, Falcón LÁ, et al. Papillary thyroid carcinoma from a thyroglossal cyst: case series. J Surg Case Rep 2022 Feb;2022(2):rjab613.