Allergic rhinitis (AR) is the most common immunological disorder, with prevalence rates reaching up to 50% in some countries. Often underestimated, AR is a global health problem that contributes to significant morbidity. In children, AR not only diminishes the quality of life (QoL) through its symptoms but also affects contiguous organs such as the sinuses, ears, and chest. Additionally, it causes sleep disturbances, leading to reduced school performance, family difficulties, and decreased participation in outdoor activities. Much of our understanding of pediatric AR epidemiology is derived from the International Study of Asthma and Allergies in Childhood survey, first conducted in 1997 and subsequently repeated.1
AR is an immunoglobulin E-mediated condition triggered by exposure of the nasal mucosa to allergens. A study among Saudi schoolchildren reported a prevalence rate of 27.1%.2 AR can lead to nasal obstruction, itching, and psychological effects such as stress, depression, and anxiety, interfering with sleep, mood, and academic performance.3 In 2023, a study conducted in Al-Ahsa demonstrated that AR significantly impacts the QoL and is associated with moderate to high stress levels.3
Several studies have explored the prevalence, patterns, and severity of AR among children and teenagers in Saudi Arabia. Alhazmi reported a prevalence rate of 51.3% for AR or symptoms indicative of AR in this demographic in the Al-Qassim region.4 In 2020, a study in Madinah examined the prevalence, knowledge, and practices regarding AR, revealing a significant proportion of the population was affected, particularly those from favorable family backgrounds.5 Additionally, a study by Albaloushi, involving 807 participants, found an increasing prevalence of AR, with 76% of participants either diagnosed with AR or exhibiting symptoms consistent with the condition.6
The literature on the impact of AR on the QoL is limited. To our knowledge, no studies have been conducted to evaluate this in Tabuk. Therefore, this study aimed to assess the prevalence and impact of AR among pediatric patients aged < 14 years.
Methods
This cross-sectional observational study was conducted from September 2023 to April 2024 in Tabuk, Saudi Arabia. The study aimed to assess the prevalence and impact of AR among pediatric patients aged < 14 years. Ethical approval was obtained from the Research Ethics Committee at the University of Tabuk. The study adhered to the Declaration of Helsinki, with informed consent appropriately obtained and participants’ privacy and confidentiality maintained. The committee issued an official approval letter (number UT-310-155-2023), which was mandatory for initiating the data collection process.
A simple random sampling method was used to estimate a sample size of 385 with a 95% confidence levels using the Qualtrics calculator, and a 50% assumed prevalence of AR, a conservative estimate given that the exact prevalence was unknown.7 This method ensured that every pediatric patient had an equal chance of being selected for the study. A comprehensive list of all eligible pediatric patients was compiled, from which 385 participants were randomly selected using random number generation techniques. This approach minimized selection bias. This sample size was chosen to ensure sufficient statistical power to detect significant associations and maintain the reliability and validity of the study findings. Ultimately, 300 participants responded, resulting in a 78.1% response rate.
The inclusion criteria included pediatric patients and their parents residing in Tabuk who consented to participate in the electronic self-administered questionnaire. Exclusion criteria included individuals who refused to participate, those living outside of Tabuk, pediatric patients with other chronic illnesses that could confound the study results, parents or guardians unable to provide informed consent, and children who had not been diagnosed with AR. Data were collected through an online structured questionnaire derived from similar previous studies.1,8–10 The questionnaire ensured anonymity and confidentiality of personal information for research purposes. The children were already diagnosed with AR by their treating physician according to the Saudi guidelines. A comprehensive statistical analysis was conducted on the dataset, encompassing descriptive and inferential methodologies. Descriptive statistics were used to summarize the demographic characteristics of the participants, including age, gender, and other relevant features. Means, medians, SD, and frequency distributions were calculated as appropriate for continuous and categorical variables.
Inferential analysis included the use of the chi-square test and multivariate logistic regression. The chi-square test was applied to assess the association between categorical variables, such as the presence of AR, and demographic characteristics like gender and age groups. This test is particularly suitable for large sample sizes, ensuring that the expected frequencies within each category are sufficiently high. Additionally, multivariate logistic regression analysis was conducted using IBM SPSS (IBM Corp. Released 2023. IBM SPSS Statistics for Windows, Version 29.0.2.0 Armonk, NY: IBM Corp.) to identify predictors and assess the strength of associations between multiple independent variables and the dependent variable, the presence of AR. The regression model incorporated factors such as age, gender, environmental influences, family history, and other relevant variables.
The significance level was set at a p-value of < 0.05, with a 95% CI. Odds ratios (ORs) with corresponding CIs were reported to quantify the strength of associations.
Results
The study initially included 300 participants, with 65 excluded based on the exclusion criteria, resulting in 235 pediatric patients. Among them, 129 (54.9%) were female and 106 (45.1%) were male. The age distribution was as follows: 70 (29.8%) were < 5 years, 98 (41.7%) were 5–10 years, and 67 (28.5%) were 11–14 years old. The majority of participants, 219 (93.2%), were Saudi nationals, with 16 (6.8%) being non-Saudi. Most of the children’s parents were married (n = 209, 88.9%), while 26 (11.1%) were widowed or divorced. The predominant level of education among fathers was a bachelor’s degree (n = 168, 71.5%), and 179 (76.2%) mothers also held bachelor’s degrees. Employment was common among fathers (n = 161, 68.5%) and mothers who were either employed (n = 124, 52.8%) or housewives (n = 68, 28.9%). Most families reported a monthly income above 10 000 SAR (n = 152, 64.7%) [Table 1].
Table 1: Sociodemographic features of participants (N = 235).
|
Sex
|
|
|
Female
|
129 (54.9)
|
|
Male
|
106 (45.1)
|
|
Age, years
|
|
|
< 5
|
70 (29.8)
|
|
5–10
|
98 (41.7)
|
|
11–14
|
67 (28.5)
|
|
Nationality
|
|
|
Non-Saudi
|
16 (6.8)
|
|
Saudi
|
219 (93.2)
|
|
Marital status of parents
|
|
|
Widowed/divorced
|
26 (11.1)
|
|
Married
|
209 (88.9)
|
|
Educational status of fathers
|
|
|
Illiterate/primary to intermediate
|
23 (9.8)
|
|
Secondary education
|
44 (18.7)
|
|
Bachelor’s degree
|
168 (71.5)
|
|
Educational status of mothers
|
|
|
Illiterate/primary to intermediate
|
14 (6.0)
|
|
Secondary education
|
42 (17.9)
|
|
Bachelor’s degree
|
179 (76.2)
|
|
Employment status of fathers
|
|
|
Employee
|
161 (68.5)
|
|
Health practice
|
23 (9.8)
|
|
Freelancer
|
17 (7.2)
|
|
Student/unemployed
|
7 (3.0)
|
|
Retired
|
27 (11.5)
|
|
Employment status of mothers
|
|
|
Employee
|
124 (52.8)
|
|
Housewife
|
68 (28.9)
|
|
Health practice
|
18 (7.7)
|
|
Freelancer
|
12 (5.1)
|
|
Student/retired
|
13 (5.5)
|
|
Monthly income, SAR
|
|
|
< 5000
|
12 (5.1)
|
|
5000–10 000
|
71 (30.2)
|
Table 2 shows various features of AR among participants. Of the 235 participants, 151 (64.3%) children had been diagnosed with AR, while 84 (35.7%) had not. The duration of symptoms varied: 55 (23.4%) children experienced symptoms for less than six months, 47 (20.0%) for 6–12 months, 25 (10.6%) for 1–3 years, and 24 (10.2%) for > 3 years. The mean age at diagnosis was 56.2 ± 33.7 months, ranging from 6–156 months. Symptom frequency varied, with 62 (26.4%) children experiencing symptoms several times a week, 45 (19.1%) less than once a week, 25 (10.6%) once a week, and 19 (8.1%) daily. Seasonal allergies were reported by 149 (63.4%) children, while 98 (41.7%) had constant allergies. Allergy testing was performed on 57 (24.3%) children, revealing a median of five allergens (IQR = 3–6), ranging from 1–15 allergens.
Table 2: Different features of allergic rhinitis among participants (N = 235).
|
Has your child been diagnosed with allergic rhinitis?
|
No
|
84 (35.7)
|
|
Yes
|
151 (64.3)
|
|
How long has your child suffered from symptoms of allergic rhinitis?
|
< 6 months
|
55 (23.4)
|
|
6–12 months
|
47 (20.0)
|
|
1–3 years
|
25 (10.6)
|
|
> 3 years
|
24 (10.2)
|
|
What is the age (in months) at which a child is diagnosed with allergic rhinitis?
|
Mean ± SD
|
56.2 ± 33.7
|
|
Range
|
6–156
|
|
How often does your child suffer from symptoms of allergic rhinitis?
|
Less than once a week
|
45 (19.1)
|
|
Once a week
|
25 (10.6)
|
|
Several times a week
|
62 (26.4)
|
|
Daily
|
19 (8.1)
|
|
Does your child suffer from seasonal allergies?
|
No
|
86 (36.6)
|
|
Yes
|
149 (63.4)
|
|
Does your child suffer from constant allergies?
|
No
|
137 (58.3)
|
|
Yes
|
98 (41.7)
|
|
Have you conducted any allergy tests on your child to determine the allergens?
|
No
|
178 (75.7)
|
|
Yes
|
57 (24.3)
|
|
Median (SD)
|
5 (2.9)
|
Figure 1 shows the severity of different symptoms of AR among participants. The severity of symptoms varied among participants. Sneezing was experienced with a mild severity by 34.0%, moderate severity by 25.1%, and severe symptoms by 17.9%. A runny nose was reported with mild severity by 33.6%, moderate severity by 26.0%, and severe symptoms by 15.7%. Nose itching was experienced with mild severity by 35.3%, moderate severity by 24.7%, and severe symptoms by 14.9%. A stuffy nose affected 30.2% with mild severity, 23.0% with moderate severity, and 16.6% with severe symptoms. Continuous tearing in the eyes was reported with mild severity by 32.8%, moderate severity by 19.1%, and severe symptoms by 14.0%.
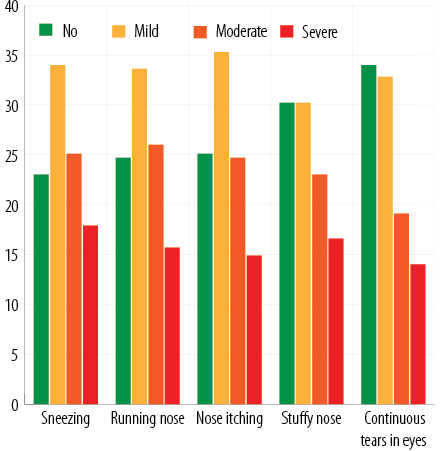 Figure 1: Degree of allergic rhinitis symptom severity.
Figure 1: Degree of allergic rhinitis symptom severity.
Table 3 evaluates the QoL among the participants, revealing varying degrees of impact on daily activities, school performance, and social interactions. Notably, 45 (19.1%) children were unaffected, while 51 (21.7%) were greatly affected. Regarding school or activity absenteeism, 61 (26.0%) children were not affected, and 64 (27.2%) were mildly affected. Symptoms experienced at school included tiredness in 123 (52.3%) children, drowsiness from nasal congestion in 49 (20.9%), learning and concentration difficulties in 42 (17.9%), and other disorders in 21 (8.9%). Sleep quality was compromised for 186 (79.1%) children, with 49 (20.9%) unaffected. General mood and emotional well-being were impacted, with 68 (28.9%) children mildly affected, 74 (31.5%) moderately affected, and 42 (17.9%) greatly affected. Emotional symptoms included anger in 41 (17.4%) children, frustration in 25 (10.6%), sorrow in 17 (7.2%), and isolation in 19 (8.1%). Physical activity restrictions were reported by 96 (40.9%) children. General enjoyment of life was unaffected in 73 (31.1%) children, mildly affected in 55 (23.4%), moderately affected in 73 (31.1%), and greatly affected in 34 (14.5%). Additionally, 101 (43.0%) parents identified environmental factors as contributors to their children’s symptoms.
Table 3: Assessment of quality of life among participants (N = 235).
|
How does allergic rhinitis affect your child’s daily activities (such as school performance and social interactions)?
|
Doesn’t affect
|
45 (19.1)
|
|
Mildly
|
62 (26.4)
|
|
Moderately
|
77 (32.8)
|
|
Greatly
|
51 (21.7)
|
|
How often does your child miss school or other activities due to symptoms of allergic rhinitis?
|
Doesn’t affect
|
61 (26.0)
|
|
Mildly
|
64 (27.2)
|
|
Moderately
|
57 (24.3)
|
|
Greatly
|
53 (22.6)
|
|
Does your child suffer from any of the following symptoms at school?
|
Tired
|
123 (52.3)
|
|
Drowsiness due to nasal congestion
|
49 (20.9)
|
|
Difficulty learning and concentrating
|
42 (17.9)
|
|
Other disorders
|
21 (8.9)
|
|
How does allergic rhinitis affect your child’s sleep quality?
|
Doesn’t affect
|
49 (20.9)
|
|
Mildly
|
60 (25.5)
|
|
Moderately
|
79 (33.6)
|
|
Greatly
|
47 (20.0)
|
|
How does allergic rhinitis affect your child’s general mood and emotional well-being?
|
Doesn’t affect
|
51 (21.7)
|
|
Mildly
|
68 (28.9)
|
|
Moderately
|
74 (31.5)
|
|
Greatly
|
42 (17.9)
|
|
Does your child suffer from any of the following symptoms?
|
Nothing
|
133 (56.6)
|
|
Anger
|
41 (17.4)
|
|
Frustration
|
25 (10.6)
|
|
Sorrow
|
17 (7.2)
|
|
Isolation
|
19 (8.1)
|
|
Does your child suffer from restrictions in participating in physical activities due to allergic rhinitis?
How does allergic rhinitis affect your child’s general enjoyment of life?
|
Yes
|
96 (40.9)
|
|
Doesn’t affect
|
73 (31.1)
|
|
Mildly
|
55 (23.4)
|
|
Moderately
|
73 (31.1)
|
|
Greatly
|
34 (14.5)
|
Table 4 presents the knowledge and practices related to the management and prevention of AR among the 235 participants. Among these, 135 (57.4%) children received treatment for AR, while 100 (42.6%) did not. During the past week, 118 (50.2%) children received no treatment, 58 (24.7%) used nasal steroids, 50 (21.3%) took oral antihistamines, and nine (3.8%) used non-steroidal nasal treatments. Parental knowledge about AR varied, with 46 (19.6%) parents being unfamiliar with the condition, 139 (59.1%) having moderate knowledge, and 50 (21.3%) being very knowledgeable. Education or counseling was provided to 112 (47.7%) children, whereas 123 (52.3%) received none. Psychological or emotional support was sought by 85 (36.2%) parents, while 150 (63.8%) did not pursue such support. Satisfaction with available support and resources was reported as follows: 30 (12.8%) parents were not satisfied, 129 (54.9%) were neutral, and 76 (32.2%) were very satisfied. Preventive measures were known by 150 (63.8%) parents.
Table 4: Knowledge about treatment, management, and prevention of allergic rhinitis (N = 235).
|
Has your child received any treatment for allergic rhinitis?
|
No
|
100 (42.6)
|
|
Yes
|
135 (57.4)
|
|
What treatment did your child receive last week?
|
Nothing
|
118 (50.2)
|
|
Local steroidal
|
58 (24.7)
|
|
Oral antihistamines
|
50 (21.3)
|
|
Local non-steroidal
|
9 (3.8)
|
|
How knowledgeable do you feel about allergic rhinitis and how to deal with it?
|
Not familiar
|
46 (19.6)
|
|
Moderate
|
139 (59.1)
|
|
Very knowledgeable
|
50 (21.3)
|
|
Has your child received any education or counseling about allergic rhinitis?
|
No
|
123 (52.3)
|
|
Yes
|
112 (47.7)
|
|
Have you sought any psychological or emotional support for your child to cope with the impact of allergic rhinitis on their quality of life?
|
No
|
150 (63.8)
|
|
Yes
|
85 (36.2)
|
|
How satisfied are you with the support and resources available to improve your child’s quality of life despite allergic rhinitis?
|
Not satisfied
|
30 (12.8)
|
|
Neutral
|
129 (54.9)
|
|
Very satisfied
|
76 (32.2)
|
Table 5 examines the association between AR and various aspects of QoL among the participants. AR significantly impacted daily activities, school performance, and social interactions (p < 0.001), with 90.2% (n = 46) of children greatly affected by these issues having AR compared to 22.2% (n = 10) of those not affected. School absenteeism was significantly related to AR (p < 0.001), with 84.9% (n = 45) of those greatly affected experiencing AR. Symptoms at school, such as tiredness (61.8%) and drowsiness (65.3%), were common among children with AR, although this was not statistically significant
(p = 0.819). Sleep quality was significantly affected (p < 0.001), with 89.4% (n = 42) of those greatly affected by poor sleep quality having AR. Emotional well-being was also significantly impacted (p < 0.001), with 88.1% (n = 37) of those greatly affected by emotional issues having AR. Emotional symptoms, including anger (n = 31, 75.4%), frustration
(n = 21, 84.0%), sorrow (n = 14, 82.4%), and isolation (n = 17, 89.5%), were significantly more prevalent among those with AR (p < 0.001). Physical activity restrictions were more common (n = 79, 82.3%) among those with AR (p < 0.001). Lastly, general enjoyment of life was significantly reduced (p < 0.001), with 91.2% (n = 31) of those greatly affected by reduced enjoyment experiencing AR.
Table 5: Association between different aspects of quality of life and allergic rhinitis.
|
How does allergic rhinitis affect your child’s daily activities (such as school performance and social interactions)?
|
Doesn’t affect
|
35 (77.8)
|
10 (22.2)
|
< 0.001 a
|
|
Mildly
|
25 (40.3)
|
37 (59.7)
|
|
|
Moderately
|
19 (24.7)
|
58 (75.3)
|
|
|
Greatly
|
5 (9.8)
|
46 (90.2)
|
|
|
How often does your child miss school or other activities due to symptoms of allergic rhinitis?
|
Doesn’t affect
|
42 (68.9)
|
19 (31.1)
|
< 0.001 a
|
|
Mildly
|
21 (32.8)
|
43 (67.2)
|
|
|
Moderately
|
13 (22.8)
|
44 (77.2)
|
|
|
Greatly
|
8 (15.1)
|
45 (84.9)
|
|
|
Does your child suffer from any of the following symptoms at school?
|
Tired
|
47 (38.2)
|
76 (61.8)
|
0.819 a
|
|
Drowsiness due to nasal congestion
|
17 (34.7)
|
32 (65.3)
|
|
|
Difficulty learning and concentrating
|
14 (33.3)
|
28 (66.7)
|
|
|
Disorder
|
6 (28.6)
|
15 (71.4)
|
|
|
How does allergic rhinitis affect your child’s sleep quality?
|
Doesn’t affect
|
34 (69.4)
|
15 (30.6)
|
<0.001 a
|
|
Mildly
|
22 (36.7)
|
38 (63.3)
|
|
|
Moderately
|
23 (29.1)
|
56 (70.9)
|
|
|
Greatly
|
5 (10.6)
|
42 (89.4)
|
|
|
How does allergic rhinitis affect your child’s general mood and emotional well-being?
|
Doesn’t affect
|
36 (70.6)
|
15 (29.4)
|
< 0.001 a
|
|
Mildly
|
28 (41.2)
|
40 (58.8)
|
|
|
Moderately
|
15 (20.3)
|
59 (79.7)
|
|
|
Greatly
|
5 (11.9)
|
37 (88.1)
|
|
|
Does your child suffer from any of the following symptoms?
|
Nothing
|
65 (48.9)
|
68 (51.1)
|
< 0.001 a
|
|
Anger
|
10 (24.4)
|
31 (75.4)
|
|
|
Frustration
|
4 (16.0)
|
21 (84.0)
|
|
|
Sorrow
|
3 (17.6)
|
14 (82.4)
|
|
|
Isolation
|
2 (10.5)
|
17 (89.5)
|
|
|
Does your child suffer from restrictions in participating in physical activities due to allergic rhinitis?
|
No
|
67 (48.2)
|
72 (51.8)
|
< 0.001 a
|
|
Yes
|
17 (17.7)
|
79 (82.3)
|
|
|
Doesn’t affect
|
43 (58.9)
|
30 (41.1)
|
< 0.001a
|
|
Mildly
|
25 (45.5)
|
30 (54.5)
|
|
|
Moderately
|
13 (17.8)
|
60 (82.2)
|
|
aChi-square test.
Table 6 examines the association between various management aspects and the prevalence of AR among the participants. Specific environmental factors did not show a significant association with AR prevalence, with OR of 1.506 (95% CI: 0.782–2.901) and a p-value of 0.221. Similarly, knowledge about AR and its management was not significantly associated with prevalence, with an exponential value of (B) (Exp(B)) of 1.439 (95% CI: 0.820–2.524) and a p-value of 0.204. However, children who received education or counseling had a significantly higher likelihood of having AR, with an Exp(B) of 2.620 (95% CI: 1.269–5.411) and a p-value of 0.009. Additionally, receiving psychological or emotional support was significantly associated with a higher prevalence of AR, with an Exp(B) of 2.349 (95% CI: 1.029–5.365) and a p-value of 0.043. Satisfaction with available resources did not show a significant association, with an Exp(B) of 0.967 (95% CI: 0.575–1.626) and a p-value of 0.898. Finally, knowledge about preventive measures did not significantly impact the prevalence of AR, with an Exp(B) of 1.303 (95% CI: 0.663–2.560) and a p-value of 0.443.
Table 6: Association between different aspects of management and allergic rhinitis prevalence.
|
Specific environmental factors
|
0.409
|
0.221
|
1.506
|
0.782
|
2.901
|
|
Knowledge about allergic rhinitis and how to deal with it
|
0.364
|
0.204
|
1.439
|
0.820
|
2.524
|
|
The child receives education/counseling
|
0.963
|
0.009
|
2.620
|
1.269
|
5.411
|
|
The child receives psychological/emotional support
|
0.854
|
0.043
|
2.349
|
1.029
|
5.365
|
|
Satisfied with the resources
|
-0.034
|
0.898
|
0.967
|
0.575
|
1.626
|
|
Knowledge about preventive measures
|
0.265
|
0.443
|
1.303
|
0.663
|
2.560
|
Exp(B): exponential value of B.
Discussion
In this study, the prevalence of AR was 64.3%, higher than the prevalence reported among schoolchildren in the Jazan region (27.1%).2 A plausible explanation might be the different age groups. A previous study conducted among children and teenagers in Qassim reported a prevalence of 51.3%, similar to our findings.4 AR significantly impacts the QoL, contributing to nasal symptoms and psychological effects such as stress and depression. According to Mou et al,11 AR adversely affects QoL and work efficiency, potentially leading to mental health issues, including depression and anxiety, in a significant percentage of patients. Additionally, Albaloushi et al,3 identified an association between AR and intermediate to high stress levels in the studied population in Al-Ahsa.
Our study indicated a higher prevalence of AR among children, at 64.3%. This rate aligns with a research conducted in environments with substantial exposure to dust, pollen, and other allergens. Similarly, Kef et al,12 reported that AR prevalence varies between 10–58.5% across different geographical regions. Interestingly, our gender distribution data showed a slightly higher prevalence among females (54.9%) than males (45.1%), contrasting with other studies. The discrepancy in gender-related prevalence could be explained by hormonal changes during puberty, gut microbiota diversity, and lifestyle factors.13
The impact of AR on daily activities, school performance, and social interactions is significant. Our study found that 21.7% of children were greatly affected, corroborating findings from previous studies that highlighted substantial impairments in daily activities and school performance due to AR. Schuler and Montejo noted that AR, the most prevalent chronic condition among children, disrupts sleep, causes daytime sleepiness, leads to school absenteeism, reduces attention (presenteeism), and results in mood disturbances and lower academic performance.14 Furthermore, our study revealed that school absenteeism was notably high, with 22.6% of children frequently missing school. This finding echoes the results of Aburiziza et al,15 who reported higher absenteeism rates among children with AR.
AR symptoms severity varied among the study participants, with sneezing, runny nose, and nasal itching being predominant. Akhouri et al,16 reported similar findings, noting common symptoms such as nasal congestion, clear rhinorrhea, sneezing, postnasal drip, and nasal pruritis.The prevalence of moderate to severe symptoms in our study aligns with observations from the Global Allergy and Asthma European Network, which also documented widespread severity among children.17 Continuous tearing from the eyes was frequently reported, highlighting its common occurrence as a comorbidity in AR.18
Sleep quality was significantly impaired among children with AR, with 79.1% experiencing disturbances. This finding is consistent with a research demonstrating that AR adversely affects sleep quality, leading to daytime fatigue and impaired cognitive function. Liu et al,19 similarly, found that AR is associated with a higher risk of daytime sleep-related dysfunctions, including difficulty waking up.
Emotional well-being was notably affected, with a substantial proportion of children experiencing emotions such as anger, frustration, sorrow, and social isolation. These emotional disturbances are in line with findings from Conway et al,20 which linked AR to various psychological issues stemming from chronic discomfort and limitations in social interactions.
Our study revealed that 57.4% of children diagnosed with AR received medication, primarily nasal steroids and oral antihistamines. This treatment approach is consistent with recommendations outlined in the Next-generation AR and its Impact on Asthma guidelines, which advocate for these medications as first-line treatments.21 However, it is concerning that 50.2% of children did not receive any treatment within the past week, suggesting potential gaps in ongoing management and follow-up care.
Parental knowledge about AR varied, with 59.1% possessing moderate knowledge levels. Education and counseling significantly increased the likelihood of receiving a diagnosis, underscoring the pivotal role of parental awareness in early detection. Similarly, Kostecka et al,22 reported higher levels of parental knowledge in families regularly visiting allergists, whereas families relying solely on regular pediatric appointments showed lower awareness levels despite their children exhibiting similar symptoms.
Psychological and emotional support emerged as crucial factors, with recipients showing a higher prevalence of diagnosed AR. This underscores the importance of a holistic approach in AR management that includes psychological support. Wang et al,23 demonstrated improved AR symptoms and enhanced QoL through combined treatment with imipramine and levocetirizine, highlighting the benefits of addressing psychological stress in AR management.
In addtion, our findings corroborate previous studies highlighting the high prevalence of AR and its significant impact on QoL, which surpasses rates observed in other countries such as Brazil. The disruptions in daily activities, school performance, and sleep underscore the complex interplay of regional and environmental factors influencing AR prevalence.
Addressing these multifaceted aspects through comprehensive management strategies is crucial for optimizing outcomes and enhancing the well-being of children affected by AR. Further research should continue to explore effective interventions that encompass both medical and psychosocial dimensions of AR care.
Despite providing valuable insights into the prevalence and impact of AR in Tabuk, our study has several limitations. The cross-sectional design restricted our ability to establish causal relationships between AR and its effects on QoL. Furthermore, reliance on self-reported data from parents introduced potential biases.
Our findings underscore the high prevalence and significant impact of AR on pediatric QoL. This highlights the necessity for targeted interventions that enhance awareness, education, and support to alleviate the burden on affected children and their families. Future research should consider longitudinal designs to better elucidate causal pathways and explore interventions aimed at mitigating the impact of AR on children’s lives.
Conclusion
Our findings highlighted the high prevalence of AR and its significant impact on the QoL in children in Tabuk, including disruptions in daily activities, school performance, and sleep. Addressing these multifaceted aspects through comprehensive management strategies is crucial for optimizing outcomes and enhancing the well-being of children affected by AR. Further research should explore effective interventions encompassing AR care's medical and psychosocial dimensions.
Disclosure
The authors declare no conflicts of interest. No funding was received for this study.
references
- 1. Sikorska-Szaflik H, Sozańska B. Quality of life in allergic rhinitis - children’s and their parents’ perspective in polish urban and rural population. Health Qual Life Outcomes 2020 Mar;18(1):64.
- 2. Mahnashi TA, Faqihi MA, Moafa AN, Basudan AA, Alhazmi MN, Khawaji AF, et al. Severity and prevalence of allergic rhinitis among school children, Jazan Region Saudi Arabia. J Family Med Prim Care 2019 Feb;8(2):663-668.
- 3. Albaloushi NN, Alyahya K. The prevalence of allergic rhinitis and its complications: a survey from Al-Ahssa, Saudi Arabia. Journal of Nature and Science of Medicine 2019 Apr;2(2):57-60.
- 4. Alhazmi W. Prevalence, pattern, and severity of allergic rhinitis among children and teenagers in Qassim Region, Saudi Arabia: a cross-sectional study. J Pharm Negat Results 2022;13(1):60-67.
- 5. Albouq NG, Julaidan RA. Prevalence, knowledge, and practice regarding allergic rhinitis among Madinah Population, Saudi Arabia, in 2019–2020. Saudi Journal of Otorhinolaryngology Head and Neck Surgery 2022;24(2):67-72.
- 6. Albaloushi NN, Alyahya K. The prevalence of allergic rhinitis and its complications: a survey from Al-Ahssa, Saudi Arabia. Journal of Nature and Science of Medicine 2019;2(2):57-60.
- 7. Calculator.net. Sample size calculator. [cited 2024 September 9]. Available from: https://www.calculator.net/sample-size-calculator.html.
- 8. Greiner AN, Hellings PW, Rotiroti G, Scadding GK. Allergic rhinitis. Lancet 2011 Dec;378(9809):2112-2122.
- 9. Meltzer EO, Nathan R, Derebery J, Stang PE, Campbell UB, Yeh WS, et al. Sleep, quality of life, and productivity impact of nasal symptoms in the United States: findings from the Burden of Rhinitis in America survey. Allergy Asthma Proc 2009;30(3):244-254.
- 10. Everhart RS, Kopel SJ, Esteban CA, McQuaid EL, Klein R, McCue CE, et al. Allergic rhinitis quality of life in urban children with asthma. Ann Allergy Asthma Immunol 2014 Apr;112(4):365-70.e1.
- 11. Mou YK, Wang HR, Zhang WB, Zhang Y, Ren C, Song XC. Allergic rhinitis and depression: profile and proposal. Front Psychiatry 2022 Jan;12:820497.
- 12. Kef K, Güven S. The prevalence of allergic rhinitis and associated risk factors among university students in Anatolia. J Asthma Allergy 2020 Nov;13:589-597.
- 13. Rosário CS, Cardozo CA, Neto HJ, Filho NA. Do gender and puberty influence allergic diseases? Allergol Immunopathol (Madr) 2021 Mar;49(2):122-125.
- 14. Schuler Iv CF, Montejo JM. Allergic rhinitis in children and adolescents. Pediatr Clin North Am 2019 Oct;66(5):981-993.
- 15. Aburiziza A, Almatrafi MA, Alonazi AS, Zatari MH, Alqouzi SA, Mandili RA, et al. The prevalence, clinical picture, and triggers of allergic rhinitis in Saudi population: a systematic review and meta-analysis. J Asthma Allergy 2022 Dec;15:1831-1849.
- 16. Akhouri S, House SA. Allergic rhinitis. StatPearls Publishing 2023 [cited 2024 September 9]. Available from: https://pubmed.ncbi.nlm.nih.gov/30844213/.
- 17. Bousquet J, Burney PG, Zuberbier T, Cauwenberge PV, Akdis CA, Bindslev-Jensen C, et al. GA2LEN (global allergy and asthma European network) addresses the allergy and asthma ‘epidemic’. Allergy 2009 Jul;64(7):969-977.
- 18. Iordache A, Boruga M, Mușat O, Jipa DA, Tătaru CP, Mușat GC. Relationship between allergic rhinitis and allergic conjunctivitis (allergic rhinoconjunctivitis) - review. Rom J Ophthalmol 2022;66(1):8-12.
- 19. Liu J, Zhang X, Zhao Y, Wang Y. The association between allergic rhinitis and sleep: a systematic review and meta-analysis of observational studies. PLoS One 2020 Feb;15(2):e0228533.
- 20. Conway AE, Verdi M, Kartha N, Maddukuri C, Anagnostou A, Abrams EM, et al. Allergic diseases and mental health. J Allergy Clin Immunol Pract 2024;12(9):2298-2309.
- 21. Bousquet J, Schünemann HJ, Togias A, Bachert C, Erhola M, Hellings PW, et al; Allergic Rhinitis and Its Impact on Asthma Working Group. Next-generation allergic rhinitis and its impact on asthma (ARIA) guidelines for allergic rhinitis based on grading of recommendations assessment, development and evaluation (GRADE) and real-world evidence. J Allergy Clin Immunol 2020 Jan;145(1):70-80.e3.
- 22. Kostecka M, Kostecka-Jarecka J, Kostecka J, Iłowiecka K, Kolasa K, Gutowska G, et al. Parental knowledge about allergies and problems with an elimination diet in children aged 3 to 6 years. Children (Basel) 2022 Nov;9(11):1693.
- 23. Wang LX, Yang ZC, Kang ZP, Di LL, Tan Y, Peng XB, et al. Improvement in psychological condition of patients with persistent moderate-severe allergic rhinitis by drug therapy combined with psychological intervention. Ear Nose Throat J 2021 Sep;100(5_suppl):684S-690S.