French in origin, the term ‘triage’ (meaning ‘to pick or sort’), is utilized in modern medical settings to refer to the preliminary assessment and stratification of the wounds or illnesses of multiple patients to determine the order in which each patient should be treated based on treatment exigency.1 The triage system was introduced in the early 1800s by Dominique-Jean Larrey, a French military surgeon under Napoleon Bonaparte. Larrey’s innovation enabled the overburdened battlefield surgeons to treat casualties according to medical urgency, regardless of nationality or military rank, and may have contributed to Napoleon’s military successes.2
Today, emergency departments (EDs) worldwide implement triage systems, but there is no universal consensus on how such systems should prioritize patients.3 Instead, individual triage systems are optimized for factors that may differ by country, region, or even between specific health institutions. Oman's healthcare systems themselves exemplify such divergence. Sultan Qaboos University Hospital (SQUH), the venue of the present study, uses the Canadian Triage and Acuity Scale. Meanwhile, hospitals under the Ministry of Health and the Armed Forces Hospital, use a modified form of Emergency Severity Ind. Efforts are on to unify these systems.
Ideally, an emergency triage system should be optimized to the characteristics and requirements of the local patient population; for example, EDs in Iran are encouraged to prepare their triage paradigm for disasters and emergencies in alignment with procurable resources, relief forces, and local conditions.3 However, in practice, many triage systems still have performance issues over various metrics.4 In busy EDs, waiting times may be long and frustrating for emergency patients. This may lead to public misconceptions which can significantly impact patient satisfaction and perceptions of quality of care.
A systematic review of 16 European and North American studies found that the triage category robustly interrelated with patient satisfaction. As more urgent cases were managed earlier, patient satisfaction level was also seen as an index of waiting time.5 A study conducted in two tertiary hospitals in Canada indicated that prolonged waiting time was the most frequent reason for patients leaving the ED without being seen (79%).6 A qualitative study in a National Health Services hospital in the UK found that most ED visitors theoretically understood the need for patient prioritization by triage.7 However, they were willing to accept prioritization only for children and patients with ‘obvious’ clinical needs, but were unclear as to the definition of the latter category.7 Other researchers have noted that many respondents did not seem to pay sufficient attention to the psychosocial and emotional needs of the patients.8 There is also a tendency for many patients to visit the ED for non-emergency needs instead of primary care facilities. The reasons given include the ready availability of advanced therapeutic and diagnostic services in ED, and a public perception that ED doctors are likely to be more empathetic and competent.9,10
Studies from different parts of the world have shown that members of the public lack fundamental knowledge regarding appropriate indications for visiting the ED and how the triage system works.7–10 Due to limited research originating from Oman and other Gulf Cooperation Council (GCC) countries,11 we aimed to investigate the public knowledge and attitudes pertaining to ED utilization and the triage process among Omani adults visiting a large tertiary hospital in Muscat, Oman.
Methods
This cross-sectional study was conducted from September to November 2019 among Omani adults attending the SQUH. Ethical approval for the study was obtained from the Medical Research and Ethics Committee of the College of Medicine and Sciences, Sultan Qaboos University (Ref. MREC #1934).
Adult (> 18 years) Omani citizens visiting the SQUH ED or outpatient departments (OPDs) during the study period were recruited sequentially by the investigators during standard working hours, using a convenience sampling strategy. Healthcare personnel (i.e., doctors, nurses, medical orderlies, paramedics, etc.) were excluded from the study. The necessary sample size needed for the study was calculated to be 520 at a 95% CI with a 5% margin of error, based on an estimated total of 15 000 ED visits per year.
The participants’ knowledge and attitudes relating to appropriate ED utilization and the triaging process used in the SQUH ED were assessed using a self-administered questionnaire which was generated in-house by the research team based on the recommended steps for new questionnaire development. Initially, an informal study was conducted asking members of the public to divulge their opinions regarding the existence of the ED triage system and its specific processes, and their responses were categorized into themes, which were used to draft questions for the main study. Five experts reviewed the themes and proposed questions, and created the first version of the questionnaire. This was piloted on 20 ED visitors and nearby residents, and the questionnaire was modified based on their responses. The finalized questionnaire comprised four sections to assess the participants’ demographic characteristics, ED visit details, and their knowledge and attitudes pertaining to appropriate ED utilization and the importance of the triage system and its specific elements.
In terms of demographic data, participants were asked to divulge their age, gender, and level of education, while ED visit information consisted of the number of prior visits and whether the participants were themselves patients or were visiting or accompanying other patients to the hospital. Knowledge of appropriate ED utilization was assessed by responses to the following question: should all non-urgent cases who come to the ED be treated in the ED, even if the services needed are available at health centers/polyclinics? Also assessed were the general understanding of the ED system at SQUH and knowledge of the triage system itself, its importance, and the factors considered for prioritization. Finally, the attitude section of the questionnaire incorporated questions to determine the participants’ preferences, reasons for seeking non-emergent ED care, how they would react if the triage decisions led to lower prioritization of their case than some later arriving patients, and their opinions regarding prolonged waiting periods as a result of the triage system.
Potential participants (Omani adults, both patients and their attenders) were approached in the waiting areas of the ED and various outpatient clinics. The purpose of the study was explained to them, and informed consent was sought. An investigator handed hard copies of the questionnaire to those who consented to participate. The investigator remained available to clarify any questions or concerns from the participants while they completed their responses.
The participants’ responses to the questionnaire items were sorted into three categories, each reflecting their level of agreement with each statement, (e.g., the options include yes/no/I don’t know or agree/disagree/neutral).
The data was analyzed using IBM SPSS Statistics (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp.). Frequency and proportions were utilized to describe the findings. Responses to various questions were presented as proportions of total responses. A chi-squared test was used to examine demographic variables which might predict the participants’ knowledge and attitude responses. A p-value of < 0.05 was considered significant.
Results
Of the 740 Omani adults (including patients and their attenders) approached during the study recruitment phase, 168 were excluded due to incomplete data or refusal to participate, resulting in 572 participants (response rate: 77.3%). The majority of participants were female (56.8%). Regarding education levels, all participants were literate enough to read and respond to the questionnaire themselves; 39.9% had a high school diploma and 34.8% had a bachelor’s degree. Most participants (71.9%) were recruited from OPDs, and the remaining 28.1% from the ED [Table 1]. Most participants (80.4%) had previously visited the ED.
Table 1: Demographic characteristics of the participants (N = 572).
|
Gender
|
|
|
Male
|
247 (43.2)
|
|
Female
|
325 (56.8)
|
|
Education level
|
|
|
Secondary school or below
|
83 (14.5)
|
|
High school diploma
|
228 (39.9)
|
|
Bachelor’s degree
|
199 (34.8)
|
|
Master’s degree
|
30 (5.2)
|
|
Doctoral degree
|
12 (2.1)
|
|
Professional degree or higher
|
15 (2.6)
|
|
Recruitment setting
|
|
|
Morning OPDs
|
411 (71.9)
|
|
Morning ED
|
51 (8.9)
|
|
Afternoon ED
|
110 (19.2)
|
|
Number of prior ED visits
|
|
|
0
|
111 (19.6)
|
|
1–2
|
226 (39.9)
|
OPD: outpatient department; ED: emergency department. *Some missing responses. Total percentages may not add up to 100%.
Only 41.8% of participants knew appropriate ED utilization, namely that non-urgent cases should not be treated in the ED if the necessary services are available in other types of health institutions [Figure 1]. Men were more knowledgeable of appropriate ED utilization (45.7%) than females (38.8%) (p = 0.005). Other demographic factors, such as education level and recruitment setting, were not associated with knowledge of ED utilization (p = 0.114 and 0.410, respectively) [Table 2]. Similar proportions of those who never visited the ED and those who had previously visited the ED either 1–2 or > 2 times (37.8% and 35.4%, respectively) thought that all non-urgent cases presented to ED ‘must’ be treated in the ED (i.e., lacked knowledge of appropriate utilization of ED services). However, the majority (51.1%) of those who had visited the ED > 2 times agreed that non-urgent cases ‘must not’ be treated in the ED compared to the other two groups (34.5% and 38.7%, respectively) (p = 0.001).
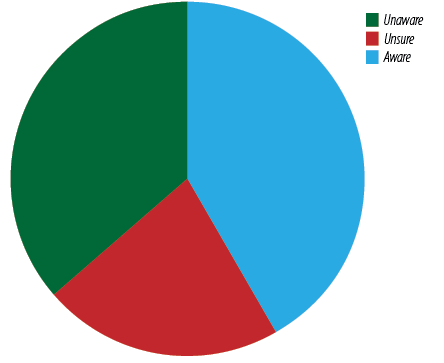 Figure 1: Frequency of knowledge regarding appropriate utilization of emergency department services among the participants (N = 572).
Figure 1: Frequency of knowledge regarding appropriate utilization of emergency department services among the participants (N = 572).
Table 2: Associations between knowledge of appropriate utilization of emergency department (ED) services and the sociodemographic characteristics of the participants (N = 572).
|
Gender
|
|
|
|
|
|
Male
|
96 (38.9)
|
38 (15.4)
|
113 (45.7)
|
0.005†
|
|
Female
|
112 (34.5)
|
87 (26.8)
|
126 (38.8)
|
|
|
Education level
|
|
|
|
|
|
High school diploma or below
|
|
|
|
|
|
Bachelor’s degree or higher
|
87 (34.0)
|
49 (19.1)
|
120 (46.9)
|
|
|
Recruitment setting
|
|
|
|
|
|
OPDs
|
152 (37.0)
|
94 (22.9)
|
165 (40.1)
|
0.410
|
|
ED
|
56 (34.8)
|
31 (19.3)
|
74 (46.0)
|
|
|
Number of prior ED visits
|
|
|
|
|
|
0
|
42 (37.8)
|
26 (23.4)
|
43 (38.7)
|
0.001†
|
|
1–2
|
84 (37.2)
|
64 (28.3)
|
78 (34.5)
|
|
OPDs: outpatient departments; *Some missing responses. Total percentages may not add up to 100%. †Statistically significant using a chi-squared test.
Overall, 55.2% of the respondents were aware of a standardized ED system for prioritizing patient care; moreover, 40.0% recognized that prioritization of care in the ED did not depend on who arrived first. Regarding their knowledge of specific factors affecting the triage process, 67.3% correctly identified vital signs as an essential metric; however, only 28.5% and 37.1% were aware that triage processes also considered the patient’s medical history and chief complaint, respectively. Regarding the importance of the triage system, most participants acknowledged that the system helped to ensure timely management of urgent cases (84.8%), reduce overcrowding in the ED (76.2%), improve the quality of care provided in the ED (80.9%), and reduce resource misutilization (68.5%) [Table 3].
Table 3: Frequency of responses to specific knowledge items concerning triage system processes and importance among the participants (N = 572).
|
In the ED, there is a system of prioritizing patient care according to standardized methods.
|
316 (55.2)
|
177 (30.9)
|
61 (10.7)
|
|
In the ED, the triage system depends on the main complaint of patients.
|
212 (37.1)
|
241 (42.1)
|
72 (12.6)
|
|
In the ED, the triage system depends on the patient’s medical history.
|
163 (28.5)
|
238 (41.6)
|
112 (19.6)
|
|
In the ED, the triage system depends on the patient’s vital signs (e.g., heart rate, blood pressure, respiratory rate, etc.).
|
385 (67.3)
|
134 (23.4)
|
26 (4.5)
|
|
In the ED, priority of treatment is always given to those who arrive first.
|
177 (30.9)
|
119 (20.8)
|
229 (40.0)
|
|
Use of the triage system helps to ensure treatment of emergency cases in time.
|
485 (84.8)
|
41 (7.2)
|
23 (4.0)
|
|
Use of the triage system helps to reduce overcrowding in the ED.
|
436 (76.2)
|
68 (11.9)
|
35 (6.1)
|
|
Use of the triage system helps to ensure the quality of care provided.
|
463 (80.9)
|
68 (11.9)
|
12 (2.1)
|
ED: emergency department. *Some missing responses. Total percentages may not add up to 100%.
In terms of attitude, the majority of participants reported that they preferred to visit the ED for non-emergent problems instead of other health institutions for various reasons, including convenience and easy access to medical care (52.4%), the quality of care received in the ED (53.1%), and the ability to receive care on the same day (59.1%). Moreover, 79.7% stated that they would accept waiting for an extended period if their situation was deemed less urgent during triage, while 48.4% would accept redirection to primary care services. When faced with prolonged waiting times, 60.3% stated that they would accept the wait and remain calm, although 26.0% stated that they would leave the hospital. Only a minority (5.2%) reported that they would consider resorting to physical or verbal abuse toward staff members if the waiting period were prolonged. When faced with a situation in which another case was prioritized over their own, 67.3% of the respondents perceived this to be justified due to medical urgency; however, 26.6% believed prioritization of the other patient to be unfair, while 17.0% attributed the situation to carelessness or error on the part of the medical staff [Table 4].
Table 4: Frequency of responses to specific attitude items concerning emergency department (ED) visit preferences and the triage system among the participants (N = 572).
|
I prefer to visit the ED (instead of HCs/PCs) for non-urgent problems because of the convenience and ease of access to medical care.
|
300 (52.4)
|
104 (18.2)
|
96 (16.8)
|
|
I prefer to visit the ED (instead of HCs/PCs) for non-urgent problems because of the quality of care received.
|
304 (53.1)
|
99 (17.3)
|
55 (9.6)
|
|
I prefer to visit the ED (instead of HCs/PCs) for non-urgent problems because of my lack of trust in the care received at HCs/PCs.
|
169 (29.5)
|
125 (21.9)
|
203 (35.5)
|
|
I prefer to visit the ED (instead of HCs/PCs) for non-urgent problems because of the ability to receive care on the same day.
|
338 (59.1)
|
100 (17.5)
|
66 (11.5)
|
|
If my condition is not deemed urgent as a result of the triage system, I would accept waiting because there are more urgent cases.
|
456 (79.7)
|
41 (7.2)
|
35 (6.1)
|
|
If my condition is not deemed urgent as a result of the triage system, I would accept redirection to a primary HC.
|
277 (48.4)
|
108 (18.9)
|
140 (24.5)
|
|
If the waiting period were prolonged because of the triage system, my response would be to remain silent and accepting.
|
345 (60.3)
|
103 (18.0)
|
81 (14.2)
|
|
If the waiting period were prolonged because of the triage system, my response would be to feel angry.
|
126 (22.0)
|
123 (21.5)
|
261 (45.6)
|
|
If the waiting period were prolonged because of the triage system, my response would be to get violent and shout at the medical staff.
|
30 (5.2)
|
40 (7.0)
|
436 (76.2)
|
|
If the waiting period were prolonged because of the triage system, my response would be to leave the hospital.
|
149 (26.0)
|
149 (26.0)
|
210 (36.7)
|
|
While you are waiting to be seen, another patient is called; you think the cause of this is because their condition is more urgent than yours.
|
385 (67.3)
|
111 (19.4)
|
37 (6.5)
|
|
While you are waiting to be seen, another patient is called; you think the cause of this is because the other patient has been unfairly prioritized.
|
152 (26.6)
|
163 (28.5)
|
192 (33.6)
|
HC: health center; PC: polyclinic. *Some missing responses. Total percentages may not add up to 100%.
Discussion
This study sought to evaluate knowledge and attitudes related to triage processes and ED utilization among Omani adults visiting a tertiary hospital in Muscat. Only 41.8% of our participants had a clear concept of appropriate ED utilization. They were aware that non-emergency cases should not be treated at EDs if the required medical services can be obtained elsewhere, for instance, local primary health centers and polyclinics. Visiting the ED for non-urgent health issues leads to overcrowding and strains the limited resources and capacity of EDs, thereby contributing to healthcare system shortcomings and adversely affecting patient outcomes and the quality of care provided.12,13
It should be noted that patients determining an ED visit as ‘unnecessary’ may vary depending on several factors including the availability and quality of appropriate primary health services. There is a need for healthcare planners and individual hospitals to evaluate local variables that may influence non-emergency ED visits and make optimal guidelines for healthcare providers and society.
Various factors affected patients’ decision-making processes when it comes to visiting the ED for non-urgent concerns. A major consideration is the cost of treatment. This can widely differ from country to country. Patients who must foot the hospital bills themselves are less likely to misuse tertiary EDs for non-emergency illnesses. For example, a major nationally representative study in the USA found that 10.1% of all ED visits to hospitals were non-emergencies.14 However, this wastage of resources is trivial compared to the corresponding figure of 87.8% revealed by a Saudi Arabian study.15 One explanation for this difference is that in the USA, healthcare is not free, causing patients to hesitate to visit expensive tertiary EDs for non-emergency services. In Saudi Arabia, medical care is free and patients can be expected to seek the best services available for all medical conditions. A similar trend can be expected in Oman and other GCC countries, as well as other countries with free, well-funded public healthcare systems.
The USA study further revealed that even among the 10.1% non-emergency visitors to ED, most had some form of health insurance, once again pointing to the cost consideration in patients’ healthcare choices. 14 An additional indication is that 87.8% of the non-emergency cases were accepted by the EDs.14 One reason for the high level of acceptance of non-emergency cases could be the profit-making model of the USA healthcare system. Our study did not focus on the proportion of non-emergency ED visits and the impact on the perceived cost of treatment. This should be included in future studies in Oman as well as other GCC countries.
There are major factors that influence patient decisions on ED utilization, such as their level of awareness of the availability of alternate resources. An American study found that this hinged on whether patients were aware of alternative sources of care or were unaware of other options and considered the ED to be the default.16 Such findings indicated that greater efforts should be made to increase public awareness of the availability and scope of alternative primary care services. Other considerations that influenced patients decision to choose between ED and primary care services included, advice from a medical professional, logistical or emotional barriers to accessing other types of care, concern over the cost of care, and overestimation of the severity of their health concern.16 Indeed, with regards to the last factor, research shows that most ED patients tend to overestimate the urgency of their medical condition and expect to be given higher priority than warranted by their actual triage categorization, particularly in the case of repeat visitors (≥ 3 ED visits in six months).17,18
Most of our participants disclosed that they preferred to visit the ED for non-emergency reasons because of convenience and ease of access (52.4%) and because they could receive care on the same day (59.1%). A Saudi Arabian study also reported most non-urgent ED visitors gave the same reasons (62% each).19Additionally, 63% of the Saudi patients revealed that they did not have a regular healthcare provider.19 Although the last factor was not assessed in the current study, it is likely to play a role in Oman as the current structure of the Omani healthcare system does not emphasize a continuity of care approach in primary care services.20
Moreover, 53.1% of our participants claimed that they preferred ED because they believed that tertiary hospitals provide higher quality care, with 29.5% reporting that they had lower trust in primary and secondary centers. Such a belief is supported by two American studies that found that patients often prefer EDs because tertiary hospitals are perceived to offer more advanced services and facilities, rapid access to care, and a belief that ED doctors are more empathetic and competent than other healthcare practitioners.9,10 It is possible that the misutilization of ED facilities for non-emergent concerns might be reduced by changes in the timing, accessibility, and content of services provided by general practitioners, which could motivate patients to reconsider defaulting to the ED for concerns that could be adequately treated at the primary care level.21 A 2010 literature review of triage systems with particular reference to Saudi Arabia recommended capacity-building and educational efforts to build up public confidence in the triage system by increasing community awareness of how patients are prioritized according to the severity of their condition, rather than as a result of other factors.11
Overall, 67.3% of participants in the present study understood that the triage decisions are based on the patient’s vital signs. This understanding may stem from their previous experiences receiving ED care. However, very few were aware that a patient’s primary complaint and medical history are also crucial for the triage process. A prospective cohort study found unusual vital signs during triage significantly correlated with unfavorable patient outcomes, including intensive care admission and in-hospital mortality.22 That study also found that including the primary complaint reported by patients in the triage process could result in over-triage, as most of their patients reported complaints that they perceived to be more urgent than what their vital signs indicated.22 This aligns with the frequent observation that ED patients tend to overestimate the severity of their health conditions.17,18
In the present study, 30.9% of participants mistakenly believed that treatment in the ED was prioritized on a ‘first come, first served’ basis. This misconception, also found elsewhere, can adversely affect patients’ acceptance of waiting times and contribute to negative perceptions. It was investigated by a two-phase study in Canada, which sought to evaluate patient expectations of ED care.23,24 In the first phase, focus group discussions were conducted among patients with and without a history of visiting the ED over the preceding year, as well as with ED staff members themselves.23 The perceptions of patients and staff differed on the need for frequent communication and patient awareness of the triage process. Both the patient groups had similar expectations of ED care, particularly with regards to the need for frequent updates and communication by ED staff; however, expectations of appropriate wait times varied, with inexperienced visitors expecting more rapid care.23 Prolonged waiting periods (≥ 3 hours) were a common concern among both patient groups, particularly in the absence of staff updates. Pertaining to the triage system, both patient groups anticipated the sickest patients to be treated first; however, inexperienced visitors desired a ‘take-a-number’ system for minor complaints, so patients might leave and return at their leisure.23
In the second phase of the research, cross-sectional telephone surveys were conducted with former ED visitors, 64.4% of whom considered that treatment priority should be given to the most critical patients, with 59.3% perceiving that medical severity should be established by a triage nurse.24 However, they also had unrealistic expectations regarding wait times, with actual length of stay being significantly longer than expected for all groups. A study of potential mediators and moderators of ED patient complaints indicated that waiting times during triage were a significant antecedent of patient satisfaction (p < 0.01).25 Other researchers have similarly shown that a considerable proportion of the public is unfamiliar with the triage process and the ED system, a situation that contributes to negative perceptions of patient ED experiences.23,26 It has been suggested that informing patients how the system works can help mitigate such perceptions.26–28 Emergency physicians and ED staff members have also indicated that much of the public do not understand the triage process unless demonstrated.23 In one study, 41% of patients in an ED waiting room wanted additional information on how the ED functions, although this information was deemed significantly less important and desirable than information related to common medical emergencies.28
Overall, 48.4% of our participants indicated that they would accept redirection to a primary health center if their condition were not deemed urgent based on the triage system. In a previous qualitative study, interviewees have similarly suggested that the triage processes might be expanded to allow for the redirection of non-urgent patients to alternative healthcare services.7 A survey of patients waiting for ED care at a public hospital in the USA reported that 38% were willing to exchange their ED visit for an OPD appointment within three days.29
In terms of attitudes regarding prolonged waiting periods as a result of the triage system, 60.3% of our participants reported that they would remain silent and accept the situation. Moreover, 45.6% disagreed that they would get angry and 76.2% opposed being violent or shouting at medical staff. Lastly, 36.7% were against leaving the hospital despite the considerable waiting period. In contrast, a study in Canada indicated that prolonged waiting time was the most frequent reason (cited by 79% of respondents) for leaving the ED without being seen.6
In contrast, 79.7% of our participants reported that they would accept longer waiting periods because of more urgent cases, as determined by the triage system. Also, when faced with a hypothetical situation where a later-arriving patient was prioritized over them, 67.3% agreed that this was likely because the latter's condition was more urgent than their own. Our respondents’ response was similar to that in phase two of the Canadian study,24 where 64.4% agreed that the most critical patients should be prioritized over themselves.
Overall, most participants in the current study were aware of the importance of the triage system, agreeing that the triage system helps to ensure timely treatment of emergency cases (84.8%), improves the quality of ED care (80.9%), reduces overcrowding in the ED (76.2%), and avoids wasting medical resources (68.5%). This consistent understanding of how the triage system positively impacts various healthcare services is an important basis for further efforts to encourage public awareness and acceptance of appropriate ED utilization in Oman.
To our knowledge, this is the first study investigating community knowledge and attitudes relating to ED visits and the triage system in Oman. In addition, the study was strengthened by the high response rate (77.3%) due to the self-administered data collection method employed and the presence of investigators during survey completion to clarify doubts. Moreover, most respondents had themselves previously experienced the triage system while seeking emergency medical care, which helps raise the credibility of our findings.
This study has some limitations. First, it was conducted in a single hospital and might not be generalizable. A second limitation was that some participants did not complete the entire questionnaire, which led to our having to exclude certain factors during the analysis, such as age, number of prior visits to the ED, and self-reported reason for visiting the ED. Finally, only a minority of the participants were recruited from EDs, while the majority was from non-emergency OPDs. This difference could have affected the accuracy of responses and data analysis.
Despite these limitations, this is a pioneering study, and its findings can provide a basis for future research. We recommend future research with a larger sample size using a more refined, standardized, and validated version of the instrument used in this study. This instrument should also have appropriate cut-off points generalizable to the Omani population. In addition, research should be conducted at multiple ED settings in various other hospitals and institutions in Oman to increase the generalizability of the findings. Furthermore, additional demographic data like age, marital status, and place of residence need to be included to determine more underlying factors affecting knowledge and attitudes pertaining to the triage system and utilization of ED services among Omani citizens.
Conclusion
Triage systems are used by EDs worldwide to prioritize patients based on case severity and treatment urgency, thereby optimizing ED resources and patient outcomes. Our findings suggest that Omani community has insufficient knowledge of the triage process and appropriate utilization of ED services. However, based on the available knowledge, their responses were positive. Therefore, it is necessary to increase the public’s basic knowledge of the triage process to improve patient satisfaction and confidence in the healthcare system.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
references
- 1. Soanes C, Hawker S, Elliott J, Fowler FG, Fowler HW, editors. Pocket Oxford English Dictionary. 10th ed. Oxford, UK: Oxford University Press; 2013.
- 2. Skandalakis PN, Lainas P, Zoras O, Skandalakis JE, Mirilas P. “To afford the wounded speedy assistance”: dominique jean Larry and napoleon. World J Surg 2006 Aug;30(8):1392-1399.
- 3. Bazyar J, Farrokhi M, Khankeh H. Triage systems in mass casualty incidents and disasters: a review study with a worldwide approach. Open Access Maced J Med Sci 2019 Feb;7(3):482-494.
- 4. Hinson JS, Martinez DA, Cabral S, George K, Whalen M, Hansoti B, et al. Triage performance in emergency medicine: a systematic review. Ann Emerg Med 2019 Jul;74(1):140-152.
- 5. Taylor C, Benger JR. Patient satisfaction in emergency medicine. Emerg Med J 2004 Sep;21(5):528-532.
- 6. Fraser J, Atkinson P, Gedmintas A, Howlett M, McCloskey R, French J. A comparative study of patient characteristics, opinions, and outcomes, for patients who leave the emergency department before medical assessment. CJEM 2017 Sep;19(5):347-354.
- 7. Cross E, Goodacre S, O’Cathain A, Arnold J. Rationing in the emergency department: the good, the bad, and the unacceptable. Emerg Med J 2005 Mar;22(3):171-176.
- 8. Gordon J, Sheppard LA, Anaf S. The patient experience in the emergency department: a systematic synthesis of qualitative research. Int Emerg Nurs 2010 Apr;18(2):80-88.
- 9. Lega F, Mengoni A. Why non-urgent patients choose emergency over primary care services? Empirical evidence and managerial implications. Health Policy 2008 Dec;88(2-3):326-338.
- 10. Vogel JA, Rising KL, Jones J, Bowden ML, Ginde AA, Havranek EP. Reasons patients choose the emergency department over primary care: a qualitative metasynthesis. J Gen Intern Med 2019 Nov;34(11):2610-2619.
- 11. Qureshi NA. Triage systems: a review of the literature with reference to Saudi Arabia. East Mediterr Health J 2010 Jun;16(6):690-698.
- 12. Rasouli HR, Esfahani AA, Nobakht M, Eskandari M, Mahmoodi S, Goodarzi H, et al. Outcomes of crowding in emergency departments: a systematic review. Arch Acad Emerg Med 2019 Aug;7(1):e52.
- 13. Morley C, Unwin M, Peterson GM, Stankovich J, Kinsman L. Emergency department crowding: a systematic review of causes, consequences and solutions. PLoS One 2018 Aug;13(8):e0203316.
- 14. Honigman LS, Wiler JL, Rooks S, Ginde AA. National study of non-urgent emergency department visits and associated resource utilization. West J Emerg Med 2013 Nov;14(6):609-616.
- 15. Alnasser S, Alharbi M, AAlibrahim A, Aal Ibrahim A, Kentab O, Alassaf W, et al. Analysis of emergency department use by non-urgent patients and their visit characteristics at an academic center. Int J Gen Med 2023 Jan;16:221-232.
- 16. Shaw EK, Howard J, Clark EC, Etz RS, Arya R, Tallia AF. Decision-making processes of patients who use the emergency department for primary care needs. J Health Care Poor Underserved 2013 Aug;24(3):1288-1305.
- 17. Ahmed N, Khan SS, Mehmood Y, Ahad B, Hussain H, Ullah N. A study on the factors associated with non- urgent utilization of emergency department. J Saidu Med Coll Swat 2001 Oct;8(2):83-89.
- 18. Toloo GS, Aitken P, Crilly J, FitzGerald G. Agreement between triage category and patient’s perception of priority in emergency departments. Scand J Trauma Resusc Emerg Med 2016 Oct;24(1):126.
- 19. Alyasin A, Douglas C. Reasons for non-urgent presentations to the emergency department in Saudi Arabia. Int Emerg Nurs 2014 Oct;22(4):220-225.
- 20. Al-Azri M, Al-Ramadhani R, Al-Rawahi N, Al-Shafee K, Al-Hinai M, Al-Maniri A. Patients’ attitudes and experiences of relational continuity in semi-urban general practices in Oman. Fam Pract 2014 Jun;31(3):303-310.
- 21. Hong M, Thind A, Zaric GS, Sarma S. The impact of improved access to after-hours primary care on emergency department and primary care utilization: a systematic review. Health Policy 2020 Aug;124(8):812-818.
- 22. Barfod C, Lauritzen MM, Danker JK, Sölétormos G, Forberg JL, Berlac PA, et al. Abnormal vital signs are strong predictors for intensive care unit admission and in-hospital mortality in adults triaged in the emergency department - a prospective cohort study. Scand J Trauma Resusc Emerg Med 2012 Apr;20:28.
- 23. Watt D, Wertzler W, Brannan G. Patient expectations of emergency department care: phase I–a focus group study. CJEM 2005 Jan;7(1):12-16.
- 24. Cooke T, Watt D, Wertzler W, Quan H. Patient expectations of emergency department care: phase II–a cross-sectional survey. CJEM 2006 May;8(3):148-157.
- 25. Abidova A, da Silva PA, Moreira S. Understanding complaints in the emergency department. Health Serv Insights 2021 Dec;14:11786329211057351.
- 26. Stuart PJ, Parker S, Rogers M. Giving a voice to the community: a qualitative study of consumer expectations for the emergency department. Emerg Med (Fremantle) 2003 Aug;15(4):369-375.
- 27. Seibert T, Veazey K, Leccese P, Druck J. What do patients want? Survey of patient desires for education in an urban university hospital. West J Emerg Med 2014 Nov;15(7):764-769.
- 28. Björvell H, Stieg J. Patients’ perceptions of the health care received in an emergency department. Ann Emerg Med 1991 Jul;20(7):734-738.
- 29. Grumbach K, Keane D, Bindman A. Primary care and public emergency department overcrowding. Am J Public Health 1993 Mar;83(3):372-378.