T raumatic cervical spine injuries in children have an estimated prevalence of 1.5%.1 Small children are particularly prone to upper cervical spine injuries, attributable to the cartilaginous endplate between the dens and body axis and the immature musculature of the cervical spine.2,3 The most common cause of injury is high-energy trauma. It is essential to distinguish such fractures from the usual anatomical variants and ossification centers. Due to the complex developmental anatomy and morphology of the C2 complex, diagnosing pediatric cervical spine injuries is challenging and sometimes missed, risking suboptimal outcome and future disability. The optimal treatment strategy for these fractures is conservative, except for displaced fractures which may require surgery.4
Brown-Séquard Syndrome (BSS) is a rare neurological condition that occurs secondary to damage to one-half of the spinal cord. Symptoms include weakness or paralysis on one side of the body, as well as loss of sensation and proprioception. An odontoid synchondrosis fracture with damage to the spinal cord on one side can cause BSS and a few such cases have been reported in adults.5 BSS associated with odontoid synchondrosis fracture requires prompt medical attention and may even require surgery to repair the fracture and relieve pressure on the spinal cord.
We report a case of undiagnosed and untreated displaced odontoid synchondrosis fracture in a toddler who later presented to us with signs and symptoms of BSS.
Case Report
A two-year-old girl was brought to our out patient department in 2022, with difficulty in moving her neck, gait abnormalities, and weakness of the right side of the body. She had a reported history of falling from bed three months earlier. The family’s lower socio-economic status was the reason for the late presentation. The child also had a concurrent complaint of urinary tract infection with urine culture showing Escherichia coli. A written consent was obtained from the patient's father.
On examination, the patient had restricted neck movement due to severe motor weakness. Her Glasgow Coma Scale score was 15/15 with decreased tone and power of 2/5 in the right upper and lower limbs. Sensory examination showed ipsilateral loss of touch, vibration, and motor and sensory functions in the right arm and right leg, with upgoing Babinski reflex. On ocular examination, eye squint was noted. Computed tomography scan and magnetic resonance imaging of the cervical spine revealed an incomplete fracture of the C2 vertebra, resulting in focal kyphosis and posterior impingement over the craniocervical junction along with significant cord thinning [Figures 1 and 2].
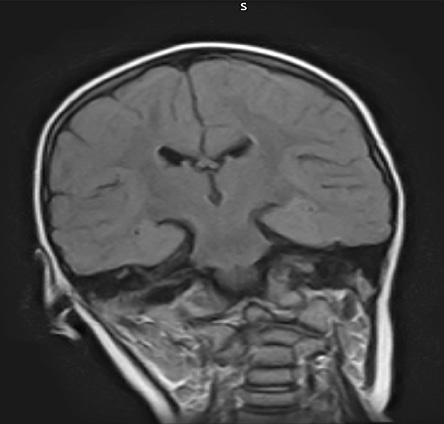 Figure 1: MRI of the cervical spine coronal section with restricted neck movement and signs of Brown- Séquard Syndrome showing abnormal rightward neck tilting due to fracture with gross asymmetry.
Figure 1: MRI of the cervical spine coronal section with restricted neck movement and signs of Brown- Séquard Syndrome showing abnormal rightward neck tilting due to fracture with gross asymmetry.
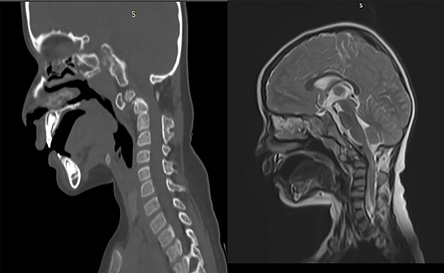 Figure 2: CT and MRI of the cervical spine sagittal section showing displaced complete fracture of odontoid process with posterior impingement at cervico-medullary junction with edema.
Figure 2: CT and MRI of the cervical spine sagittal section showing displaced complete fracture of odontoid process with posterior impingement at cervico-medullary junction with edema.
The patient was immobilized and placed in a cervical collar to prevent further damage to the spinal cord. Intravenous antibiotics were administered to treat the urinary tract infection, and she was started on a course of corticosteroids to reduce inflammation and prevent further damage to the spinal cord. Surgical intervention was discussed, but in view of her age and the incomplete nature of the fracture, a conservative approach was taken, and she underwent immobilization in a cervical collar for an extended period.
Subsequently, the patient was referred to a physical therapy program to manage the abnormalities in gait and motor function. Regular follow-up appointments were scheduled to monitor her progress, and a multidisciplinary approach was taken to provide comprehensive care.
Discussion
Cervical spine injuries are rare in children. Among those, upper cervical spine injuries are the most common due to the elasticity of the pediatric ligaments and the immature musculature around that area. C2 is the most commonly injured area in children younger than seven due to incompletely fused synchondroses in early childhood. The increased vulnerability in these ages can be attributed to the sub-dental synchondroses fusion by the age of five, which disappears only by around 9–10 years.2,6 While most cases present without neurological deficits, any missed and untreated injury can lead to malunion resulting in multiple complications ranging from transient paresthesia to complete paralysis. If the spinal cord is also involved, it most commonly presents with central cord-type syndrome.7 A few odontoid fracture cases with associated BSS have been reported in adults, but only one in the pediatric age group.8
BSS occurs due to disruption of the descending lateral corticospinal tract, dorsal column, and spinothalamic tract which leads to peculiar findings of ipsilateral motor weakness, loss of vibration and proprioception, with contralateral loss of pain and temperature. These injuries can be easily missed on the first presentation as their subtle nature may cause the clinician to miss or underestimate the injury. A study on 15 pediatric odontoid fracture cases found that 35% of the fractures were initially misdiagnosed due to not performing appropriate radiographic imaging.7 Therefore, young children who have suffered high-energy trauma and present with neck symptoms should be thoroughly reviewed for synchondroses fractures to avoid delayed diagnosis and the consequent neurological sequelae.
The first line treatment for odontoid synchondrosis fracture is immobilization via Halo vest, Minerva cast, or soft collar, depending on the surgeon’s judgment.9 Cases that do not heal with conservative management and those presenting with malunion, non-union, and secondary neurological complications may need surgical correction.10 Odontoid fractures being very uncommon, with limited cases reported, treatment options are often debatable. For example, a patient who presented with neurological complications secondary to dislocated fractures was subjected to transoral reduction and open posterior instrumentation, leading to significant improvement.11
Even though the present case was presented to us late, conservative management followed by physiotherapy was successful. Other patients may not be so fortunate. We strongly suggest including BSS in the differential diagnosis of neck pain and neurologic symptoms in children who have suffered high-energy trauma.
Perhaps the extreme scarcity in the literature of cases of pediatric BSS associated with odontoid synchondrosis might be in part due to missed diagnoses. If so, more cases might be reported in the future as awareness of this condition grows, and advanced imaging techniques are increasingly used in suspected cases, leading to better understanding, management, and positive outcomes for the affected children.
Conclusion
The occurrence of odontoid fracture complicated by BSS is rare in pediatric patients, and only one case has been previously reported in the literature. Due to angulation, odontoid fractures can be missed on initial X-ray images leading to delay in diagnosis and treatment such as in our patient. We recommend that all children presenting with neck symptoms after high energy trauma should be thoroughly reviewed for these fractures. Supportive management is the mainstay for uncomplicated fractures. Surgery may be considered if there is any displacement or neurological complication.
Disclosure
The authors declared no conflicts of interest.
references
- 1. Patel JC, Tepas JJ III, Mollitt DL, Pieper P. Pediatric cervical spine injuries: defining the disease. J Pediatr Surg 2001 Feb;36(2):373-376.
- 2. Leonard JR, Jaffe DM, Kuppermann N, Olsen CS, Leonard JC; Pediatric Emergency Care Applied Research Network (PECARN) Cervical Spine Study Group. Cervical spine injury patterns in children. Pediatrics 2014 May;133(5):e1179-e1188.
- 3. Subach BR, McLaughlin MR, Albright AL, Pollack IF. Current management of pediatric atlantoaxial rotatory subluxation. Spine (Phila Pa 1976) 1998 Oct;23(20):2174-2179.
- 4. Razii N, Sharma A, Ahuja S. Complete remodelling of a displaced odontoid synchondrosis fracture managed conservatively: a case report. J Pediatr Orthop B 2019 Jul;28(4):411-414.
- 5. Wu YT, Ho CW, Chang ST, Chen LC. Brown-Sèquard syndrome caused by type III odontoid fracture: a case report and review of the literature. Spine (Phila Pa 1976) 2010 Jan;35(1):E27-E30.
- 6. Gebauer M, Lohse C, Barvencik F, Pogoda P, Rueger JM, Püschel K, et al. Subdental synchondrosis and anatomy of the axis in aging: a histomorphometric study on 30 autopsy cases. Eur Spine J 2006 Mar;15(3):292-298.
- 7. Odent T, Langlais J, Glorion C, Kassis B, Bataille J, Pouliquen JC. Fractures of the odontoid process: a report of 15 cases in children younger than 6 years. J Pediatr Orthop 1999;19(1):51-54.
- 8. Song KJ, Chang BS, Lee KB. Pediatric odontoid fracture causing Brown-Sequard syndrome: a case report. Acta Orthop Belg 2012 Jun;78(3):405-408.
- 9. Kim W, O’Malley M, Kieser DC. Noninvasive management of an odontoid process fracture in a toddler: case report. Global Spine J 2015 Feb;5(1):59-62.
- 10. Fassett DR, McCall T, Brockmeyer DL. Odontoid synchondrosis fractures in children. Neurosurg Focus 2006 Feb;20(2):E7.
- 11. Karamian BA, Campbell ST, Rinsky LA. Complete atlantoaxial dislocation after odontoid synchondrosis fracture: a 2-year follow-up study: a case report. JBJS Case Connect 2019;9(2):e0327.